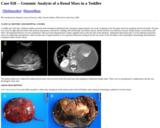
(This case study was added to OER Commons as one of a batch of over 700. It has relevant information which may include medical imagery, lab results, and history where relevant. A link to the final diagnosis can be found at the end of the case study for review. The first paragraph of the case study -- typically, but not always the clinical presentation -- is provided below.)
The patient is a 48 year old Caucasian male with a past medical history of hypertension, gastroesophageal reflux disease, irritable bowel syndrome, chronic headaches, anxiety, depression, chronic low back pain secondary to spinal stenosis status post L3 through L5 laminectomies in 2009, and end-stage osteoarthritis in bilateral hips status post total left hip (March) and total right hip (September) arthroplasties with metal-on-metal prostheses in 2008. The patient worked in the construction industry for many years and performed daily tasks that resulted in his chronic hip disease, including heavy lifting and prolonged kneeling. Following the left hip replacement, his pain was vastly improved and he did well with no complications. However, following the right hip replacement, he noted increased bilateral hip pain, right more than left. In April 2012, he presented to an outpatient clinic with these complaints, in addition to complaints of increasing confusion, headaches, blurry vision for about two weeks, and short-term memory loss. Radiologic imaging was performed at that time, but failed to reveal signs of joint failure. Interestingly, a blood cobalt level was drawn and returned 11.4 µg/L (reference range: <1.8 µg/L). He subsequently underwent a revision of the right hip in October 2012, replacing the metal-on-metal joint with a non-metal surface prosthesis. A repeat blood cobalt level was drawn after the surgery and returned 5 µg/L. He remained clinically stable following the right hip revision, but in February 2013 he presented to an outside hospital after he sustained a traumatic fall in his basement. He attributed the fall to symptoms of progressive cognitive decline, including confusion, lethargy, short-term memory loss, and depression, which he noted had worsened since his hip procedures in 2008. Computed tomography (CT) and magnetic resonance imaging (MRI) scans of the head did not reveal significant acute pathology, an electroencephalogram (EEG) was also negative for seizure-like activity or any other pathologic activity in the brain, and all other work-ups were essentially negative. On admission to the hospital, he stated that he had a history of elevated blood cobalt levels, but the patient's previous laboratory studies were not available for review by his clinicians. A repeat blood cobalt level was drawn during his hospitalization and returned 3.1 µg/L. The patient was eventually discharged from the hospital with follow-up at an outpatient toxicology clinic for further evaluation.